Guest Post by Dr. Kevin Passero
In my early 20s, I went to the doctor suddenly with this horrible pain in my chest – it felt like there was a candle burning in the top of my stomach. I had no idea what it was at first, but it became the first of many bouts of acid reflux. I took acid blockers at first, but managed to get myself off them by learning over the course of 3 years more about what’s really going on in your body.
To this day I use some of the tricks you’ll learn in this blog post below – enjoy this important knowledge.
-Dave
Acid reflux, commonly referred to as Gastro-Esophageal Reflux Disease (GERD), affects about one-third of today’s American population. It’s no surprise that pharmaceutical sales are booming at a whopping $10 billion annually[i], currently making GERD the most expensive GI disorder in America!
Nexium, AstraZeneca’s blockbuster reflux medication, ranked as the number two best selling drug of 2014, racked up sales of roughly $19.3 million dollars.[ii] Factor in the over the counter, generic, and other reflux blocking medication sales, and you can see how profits jumped to $10 billion.
Ouch.
Cleary something isn’t working. This post covers common misconceptions around acid reflux, the problems with common acid reflux medications, and what you can try instead.
So What Is Acid Reflux Really?
One of the biggest misconceptions I encounter from patients about acid reflux is that it results from having too much stomach acid.
This is what we’re told by the companies who want to sell us medications that block the production of acid by the stomach. Most people who take an acid blocking drug do get relief, so the logic seems reasonable.
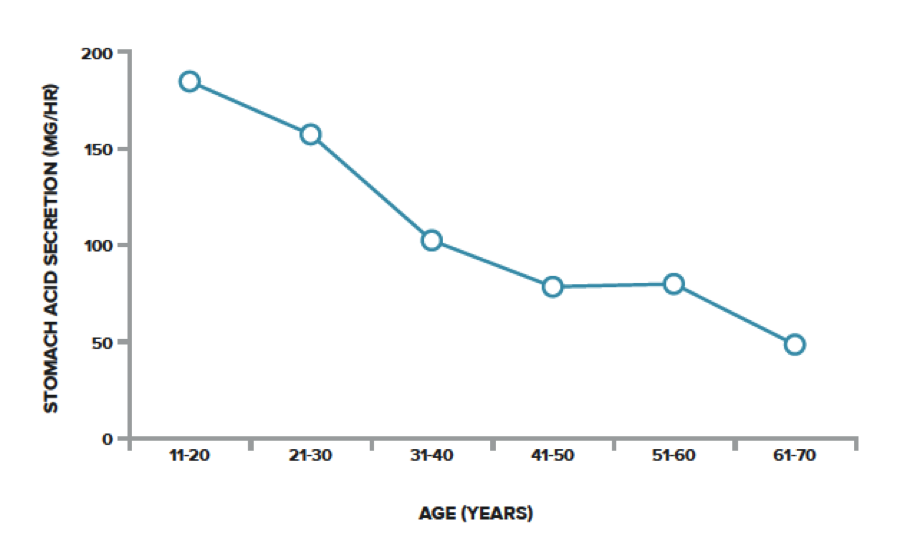
However, in most situations, nothing could be further from the truth. Most acid reflux sufferers have far too little stomach acid. The fact is, research has shown that stomach acid secretion declines sharply as we age[iii], and acid reflux becomes more common as people get older. Additional research proves the relationship between lower amounts of stomach acid and higher rates of acid reflux.[iv]
That means people with more stomach acid are less likely to develop symptoms of acid reflux.
Figure 1: Mean stomach acid secretion from the second to the eighth decade.
(Source: Why Stomach Acid Is Good for You, Wright, 2001. p.20)
According to Jonathan Wright, M.D., author of Why Stomach Acid Is Good For You, “When we carefully test people over age forty who’re having heartburn, indigestion and gas, over 90% of the time we find inadequate acid production by the stomach.” This creates quite a paradigm shift in thinking!
To fully comprehend how low stomach acid can cause reflux, let’s take a brief look at how our digestive system is designed.
How The LES and Anatomy of the Esophagus Work
The lower esophageal sphincter (LES) is a band of muscle that wraps around the esophagus where it enters the stomach, and has the primary job of keeping stomach contents (food and acid) from entering the esophagus.
The tone of this muscle plays a large role in its ability to keep acid contained to the stomach, and the determining factor of how well it functions is the amount of acid present in the stomach. A highly acidic environment in the stomach will trigger that muscle to become very tight and restrict the flow of acid into the esophagus. Conversely, when stomach acid drops, the muscle loosens up, and acid can more easily enter the esophagus. This explains why low stomach acid can be a major cause of acid reflux symptoms.
Also important to understand, the cells of the stomach and esophagus are very different. While the stomach is designed to withstand acid secretions, the esophagus is not. The tiniest amount of acid, even dilute acid, in the esophagus can trigger massive amounts of acid reflux discomfort.
The Problem with Low Stomach Acid – The Drugs Are Making It Worse
Understanding that acid reflux is often the result of too little stomach acid, it’s logical that further suppression of acid is not fixing the problem and can lead to other health concerns.
Decreased absorption of important nutrients including iron, B12, and zinc have all been linked to low stomach acid.[v] [vi] [vii]
Also, acid-blocking medications actually increase the risk of developing bacterial overgrowth in the stomach since stomach acid is one of our immune barriers[viii]. Extensive research has demonstrated an increased risk of developing food allergies, drug sensitivities and certain autoimmune diseases with the use of acid-blocking medications like proton-pump inhibitors and H2 blockers.[ix] [x] [xi] [xii] [xiii]
Acid Reflux Treatment Medications are Dangerous!
Over the counter availability of acid reflux medications encourages the misconception amongst sufferers that these drugs are perfectly safe. Those who are given prescriptions from their doctor often have open ended refills, and are not warned of the side effects and risks associated with long-term use. Many of my new patients report use of acid-blocking medication for 10+ years!
4 Extremely Serious Side Effects of Acid-Blocking Medications
-
#1: Increased Bone Fracture Risk:
Considering the epidemic rates of osteoporosis in our country today, this well-documented side effect from long-term use of acid-blocking medication is extremely troubling. Few doctors are talking to their patients about the risk of acid-blocking medication in relation to bone health. The FDA has even recognized this significant risk. Mandated label changes now require both prescription and over the counter acid-blocking medications to carry a warning stating the increased risk of bone fracture associated with high doses and/or long-term use of these medications.
Here is an excerpt from the 2010 safety announcement directly from the FDA website www.fda.gov
Safety Announcement [05-25-2010] The U.S. Food and Drug Administration (FDA) is revising the prescription and over-the-counter (OTC) labels for a class of drugs called proton pump inhibitors to include new safety information about a possible increased risk of fractures of the hip, wrist, and spine with the use of these medications.The new safety information is based on FDA’s review of several epidemiological studies that reported an increased risk of fractures of the hip, wrist, and spine with proton pump inhibitor use.
Some studies show that risk of bone fracture can even triple with long-term use.[xiv] Other studies, like one published in the Journal of the American Medical Association in 2006, have shown an increased risk of hip fracture with PPI therapy lasting more than 1 year.[xv]
-
#2: Increased Risk of Serious Infection
Users of acid blocking medication are at higher risk for two very dangerous, potentially fatal types of infection: pneumonia and Clostridium difficile (C. difficile).
In the May 2009 Issue of the Journal of the American Medical Association, a Harvard based researcher reported a 30% increased risk of hospital-based pneumonia in patients on proton-pump inhibitors when admitted to the hospital[xvi]. The study was based on the review of 64,000 patient records, and the researchers estimate that PPIs account for 180,000 cases of hospital acquired pneumonia and 33,000 deaths annually!
These numbers are staggering and highlight the scary truth that “properly prescribed” pharmaceutical medications fall somewhere between the first and fourth leading cause of death in the United States. This particular study was done on PPIs, but the other common class of acid-blocking medications, H2 blockers, has also been shown to increase rates of pneumonia, particularly in the elderly.
- C. difficile is a gastrointestinal infection that causes severe diarrhea and often becomes a life-threatening illness in older people. C. difficile is the most common hospital acquired infection (currently surpassing MRSA), and 90% of cases are contracted due to the administration of antibiotics disrupting the natural flora of the gut, providing C. difficile with an opportunity to thrive.
Each year, more than 28,000 people die of C. difficile infections, with almost all cases being contracted in a hospital, just after leaving a hospital or in a nursing home. C. difficile is notoriously difficult to treat, and roughly 20% of people will have a single recurrence or multiple recurrences even after aggressive treatment with antibiotics. For these reasons, C. difficile is very expensive to manage, with the average case costing somewhere between $4,000 to $9,000 in total treatment costs. Our healthcare system spends an estimated $3.8 billion every year treating these infections.
Data published in the March 2012 edition of the Journal of Clinical Gastroenterology and Hepatology looked at over 200,000 cases from 30 different studies done between 1994 and 2010. The authors found what many prior studies have already shown: “PPI therapy is associated with a twofold increase in risk for a Clostridium difficile infection.”[xvii]
-
#3: Vitamin and Mineral Deficiencies
As I discussed earlier, it has been well established that acid-blocking therapies inhibit the absorption of critical vitamins and minerals, such as iron and vitamin B12. Acid is needed to cleave these nutrients from our food for the body to absorb. Vitamin B12, in particular, is a key nutrient for the neurological system, and B12 deficiencies in elderly patients are associated with higher risk of dementia and cognitive declines.
The FDA issued a warning in 2011 notifying healthcare practitioners and the public that long-term use of acid-blocking medications can result in magnesium deficiency. Magnesium is the most abundant mineral in the body and an essential co-factor for running the enzymatic reactions necessary for proper cell function.
-
#4: Rebound Symptoms and Addiction
On top of everything else, the body becomes dependent on the acid-blocking drug. When the reflux medication is discontinued, elevated levels of the stomach hormone, gastrin, trigger a massive production of acid in the stomach, and reflux symptoms tend to flare up.
A double-blind placebo-controlled trial involving 48 individuals published in the American Journal of Gastroenterology concluded that a 4 week course of proton pump inhibiting medications caused acid reflux symptoms, even in previously asymptomatic individuals, when the medication was discontinued.[xviii]
It took about three weeks for the rebound effects to wear off. Another double-blind placebo-controlled trial involving 120 healthy volunteers found that PPI therapy for 8 weeks induces acid-related symptoms in healthy people after withdrawal.[xix]
How to Biohack your system to eliminate acid reflux without drugs:
-
Avoid Food Allergies:
Most people are already aware that eating certain foods can worsen reflux symptoms. Acidic foods like tomatoes and citrus fruits, and spicy foods, irritate an already inflamed surface of the esophagus and stomach. Foods high in fat slow stomach emptying, increasing upward pressure on the lower esophageal sphincter and increasing the chances that food and acid will reflux upwards. Highly acidic or spicy foods combined with dietary fat are a bad combination for reflux sufferers!
In my experience, the bigger issue that connects foods to reflux is food allergy. I am not referring to the stereotypical hive or lip swelling reaction that is the result of a classic IgE mediated food reaction. I am referring to a delayed sensitivity reaction, which is mediated by a different arm of the immune system. These reactions can take 3-4 days to manifest and are responsible for causing chronic, ongoing states of inflammation and irritation throughout the body. They can be responsible for brain fog, joint pain, irritable bowel symptoms, skin conditions, and most certainly reflux.
The two most notable foods to cause a reflux problem are gluten and dairy.
These foods are highly inflammatory, and I have seen many people completely solve their reflux riddle by eliminating them. For maximum results, I recommend that people try a 4 week elimination of these foods when starting a reflux recovery program. After 4 weeks, they can be added back in, one at a time, for a more definitive answer regarding their possible role in reflux symptoms. Other foods may also be of concern, but gluten and dairy are the most likely culprits.
-
Use the natural reflux cures provided by nature:
There are several natural substances that work with the body to heal irritated tissue and support optimal gastrointestinal function. These tools are often the key to reversing and managing reflux without resorting to dangerous acid suppressing medications.
Deglycrrhizinated Licorice (DGL): Of all the agents from the natural pharmacy for acid reflux, I count deglycrrhizinated licorice the most important. DGL has the ability to restore the integrity of the esophageal, stomach, and intestinal lining. It works by increasing the secretion of the protective mucus that lines our upper and lower GI tract. Mucus is one of the body’s most powerful antidotes to acid, and increasing secretions can dramatically reduce reflux irritation without having to suppress acid.
Research has shown promising results using DGL to treat stomach and small intestine ulcers. One double-blinded study compared the benefits of DGL to the acid suppressing drug, cimetidine, in the treatment of stomach ulcers, and found that both treatments worked equally when evaluated at both 6 and 12 weeks of therapy.[xx] Other clinical trials have demonstrated the benefits of DGL for stomach ulcers including one 4 week trial that showed a statistically significant reduction in ulcer size for a DGL preparation vs. a placebo.[xxi]
Mastic Gum: This resinous extract from the mastic tree (Pistacia lentiscus) has been long used in the treatment of gastric and intestinal ulcers. A publishing in the New England Journal of Medicine found that mastic gum had the ability to kill seven different strains of H. pylori in a laboratory setting.[xxii] Most impressive is several of these strains were proven to be completely resistant to the antibiotics typically used to treat H. pylori.
Mastic gum has strong anti-inflammatory properties and, like DGL, helps to soothe the irritated tissue of the stomach and esophagus allowing healing and recovery.
Other supplements for reflux include zinc carnosine, aloe leaf extracts (the non-laxative type), slippery elm bark and marshmallow root.
-
Stimulate Digestion:
Increasing stomach acid secretion improves digestion and aids your body to extract maximum amounts of nutrients from your food. There are several ways to naturally increase stomach acid.
Betaine HCL: This is supplemental hydrochloric acid, the same acid your body naturally produces in the stomach. Individuals with a diagnosed stomach or intestinal ulcer, should not use HCL supplements until the ulcer is healed. Those taking certain medications like corticosteroids (prednisone) and/or anti-inflammatory drugs such as ibuprofen, aspirin or other prescription or over the counter NSAID’s should not use HCL supplements unless under the supervision of an experienced physician. In addition, for some with moderate to severe reflux, betaine HCL can be slightly irritating at the beginning of treatment. If that is the case, use DGL and mastic gum for 2 weeks before adding HCL.
Taking supplemental HCL will return your stomach acid levels to optimal, which, in turn, results in a tightening of the lower esophageal sphincter and less acid making its way back up to the esophagus. Although there are not clinical trials proving the effectiveness of using HCL supplements for reflux, thousands of patients have achieved reflux relief and improved health by using this natural cure.
How to take HCL: To minimize side effects, it is recommended to start with one 650mg capsule of HCL w/ pepsin in the early part of each meal. If there is no discomfort or irritation after two or three days, increase the dose to two capsules at the beginning of meals. The idea is to keep increasing the dose gradually by 1 capsule every 2-3 days until you find a dose that causes a mild burning sensation. At that point, reduce the dosage to the previous number of capsules that did not cause any burning and stay at that dosage. The dose may change over time so just adjust the amount of capsules you are taking up or down.
Bitters: This is the oldest form of supporting digestion and stomach acid secretion. Bitter tasting herbs like gentian, dandelion root, and burdock root naturally stimulate digestive secretions including stomach acid. They are slightly gentler on the system and better suited at the initiation of treatment for those suffering from a lot of acid irritation.
What’s The Takeaway Here?
Acid reflux is a serious concern that causes sufferers a lot of misery. Using medications to suppress stomach acid results in reduced health and significant side effects that can be life threatening.
If you suffer from acid reflux and want to be symptom free, I encourage you to read my newly released book, The Drug Free Acid Reflux Solution.
It provides an in-depth look at everything I just covered, and gives specific recommendations to safely get off of your reflux medications and onto my natural program developed from years of clinical experience. I include my 30 day reflux recovery cookbook with recipes and meal planning ideas to make the program as simple as possible to follow. Readers are reporting relief in as little as one week and my patients have said the same.
Thankfully, with a proper diet and the right support from the natural pharmacy, most people can be reflux free without medication and actually enjoy thriving health!
References
[expand title=”Click to read the complete list of references.” swaptitle=”Click to hide references.”]
[i] American Gastroenterological Association. The Burden of Chronic Gastorintestinal Diseases Study. 2001
[ii] Medscape.com
[iii] Krasinski SD, Russell RM, Samloff IM, et al. Fundic atrophic gastritis in an elderly population. Effect on hemoglobin and several serum nutritional indicators. J Am Geriatr Soc. 1986 Nov;34(11):800-6.
[iv] Ayazi S1, Leers JM, Oezcelik A, Abate E, et al. Measurement of gastric pH in ambulatory esophageal pH monitoring. Surg Endosc. 2009 Sep;23(9):1968-73.
[v] Skikne BS, Lynch SR, Cook JD. Role of gastric acid in food iron absorption. Gastroenterology. 1981 Dec;81(6):1068-71.
[vi] Saltzman JR1, Kemp JA, Golner BB, Pedrosa MC, Dallal GE, Russell RM. Effect of hypochlorhydria due to omeprazole treatment or atrophic gastritis on protein-bound vitamin B12 absorption. J Am Coll Nutr. 1994 Dec;13(6):584-91.
[vii]Sturniolo GC1, Montino MC, Rossetto L, Martin A, D’Inca R, D’Odorico A, Naccarato R. Inhibition of gastric acid secretion reduces zinc absorption in man. J Am Coll Nutr. 1991 Aug;10(4):372-5.
[viii] Theisen J1, Nehra D, Citron D, Johansson J, Hagen JA, Crookes PF, DeMeester SR, Bremner CG, DeMeester TR, Peters JH. Suppression of gastric acid secretion in patients with gastroesophageal reflux disease results in gastric bacterial overgrowth and deconjugation of bile acids. J Gastrointest Surg. 2000 Jan-Feb;4(1):50-4.
[ix] Diesner, S. C.; Knittelfelder R (6 November 2008). “Dose-dependent food allergy induction against ovalbumin under acid-suppression: A murine food allergy model”.Immunology Letters 121 (1): 45–51.
[x] Untersmayr, Eva; Noémi Bakos (25 January 2005). “Anti-ulcer drugs promote IgE formation toward dietary antigens in adult patients”. The FASEB Journal 19 (6): 656–8.
[xi] Lebwohl, B; Spechler, SJ; Wang, TC; Green, PH; Ludvigsson, JF (September 12, 2013). “Use of proton pump inhibitors and subsequent risk of celiac disease”. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver 46 (1): 36–40.
[xii] Untersmayr, E; Schöll I (September 2003). “Antacid medication inhibits digestion of dietary proteins and causes food allergy: a fish allergy model in BALB/c mice”. The Journal of allergy and clinical immunology 112 (3): 616–623.
[xiii] Schöll, I; Untersmayr E (January 2005). “Antiulcer drugs promote oral sensitization and hypersensitivity to hazelnut allergens in BALB/c mice and humans”. The American journal of clinical nutrition 81 (1): 154–160
[xiv] Targownik LE, Lix LM, Metge CJ, Prior HJ, Leung S, Leslie WD. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ. 2008 Aug 12;179(4):319-26.
[xv] Yang YX1, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006 Dec 27;296(24):2947-53.
[xvi] Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA. 2009 May 27;301(20):2120-8.
[xvii] Deshpande A1, Pant C, Pasupuleti V, Rolston DD, Jain A, Deshpande N, Thota P, Sferra TJ, Hernandez AV. Association between proton pump inhibitor therapy and Clostridium difficile infection in a meta-analysis. Clin Gastroenterol Hepatol. 2012 Mar;10(3):225-33.
[xviii] Niklasson A1, Lindström L, Simrén M, Lindberg G, Björnsson E. Dyspeptic symptom development after discontinuation of a proton pump inhibitor: a double-blind placebo-controlled trial. Am J Gastroenterol. 2010 Jul;105(7):1531-7.
[xix] Reimer C1, Søndergaard B, Hilsted L, Bytzer P. Proton-pump inhibitor therapy induces acid-related symptoms in healthy volunteers after withdrawal of therapy. Gastroenterology. 2009 Jul;137(1):80-7, 87.
[xx] Morgan AG, McAdam WA, Pacsoo C, Damborough A. Comparison between cimetidine and Caved-S in the treatment of gastric ulceration, and subsequent maintenance therapy. Gut 1982;23:545-551
[xxi] Turpie AG, Runcie J, Thomson TJ. Clinical trial of deglycyrrhizinized liquorice in gastric ulcer. Gut 1969;10:299-302.
[xxii] Mastic Gum Kills Helicobacter pylori. N Engl J Med 1998; 339:194
[/expand]
Dr. Kevin Passero graduated from the National College of Naturopathic Medicine in Portland, Oregon, one of eight accredited naturopathic medical schools in North America. He brings cutting edge natural and holistic therapies to his patients, and provides education on the value of naturopathic medicine across the country. His practice focuses on uncovering why the body is in distress and finding the solutions necessary to restore optimal health.
Dr. Kevin Passero also hosts The Essentials of Healthy Living radio show and is the author of The Drug Free Acid Reflux Solution. You can learn more about his practice and read his blogs by visiting www.greenhealingnow.com.