[tldr]
- If you’re having symptoms and you think something’s up with your thyroid, or if you had some thyroid testing done and you want to understand the results, you might be confused on where to go from here.
- Hypothyroidism symptoms include fatigue, loss of libido, hair loss, and more.
- Hyperthyroidism symptoms include anxiety, heart palpitations, feeling hot all the time, and more.
- Typical doctors don’t run the right tests. Find out why the testing can get confusing and what to request from your doctor.
- Traditional thyroid treatment includes thyroid medication, surgery, or radiation. You might have some natural alternatives to explore.
- Read on to find out what to test, how to approach treatment, and what it all means.
[/tldr]
Until my mid-twenties, I felt like my gas pedal was all the way to the floor, and I was going slower, not faster. I was tired all the time, and doing everyday things felt like wading through a big tub of sludge.
I knew I wasn’t thinking as clearly and getting as much done as I could be. It made me feel like a failure. I wondered what was wrong with me, like I didn’t want it enough or that I should only try harder.
When I was 26, I went to an anti-aging doctor who ran a head-to-toe workup on me, which included a full thyroid panel. The tests clearly showed why I felt like crap. I didn’t have nearly enough thyroid hormone. Without it, your mitochondria, the microscopic power plants in your cells, can’t make energy. I went home with a prescription for thyroid medication.
Literally, the next day, I got my mojo back. Everything in my life felt like it took less work. I moved more quickly, I could think more clearly. The difference was like falling asleep in Kansas and waking up in technicolor Oz.
Here’s the kicker — a normal doctor would have told me my thyroid was fine. My TSH numbers were normal, and typical doctors don’t go any further than that. So, I wanted to write the guide I wish I’d had when I was falling asleep in my 12th cup of coffee of the day.
If you’re having thyroid symptoms and you think something’s up with your thyroid, or if you had some thyroid testing done and you want to understand the results, keep reading to understand where to go from here.
What does your thyroid do?
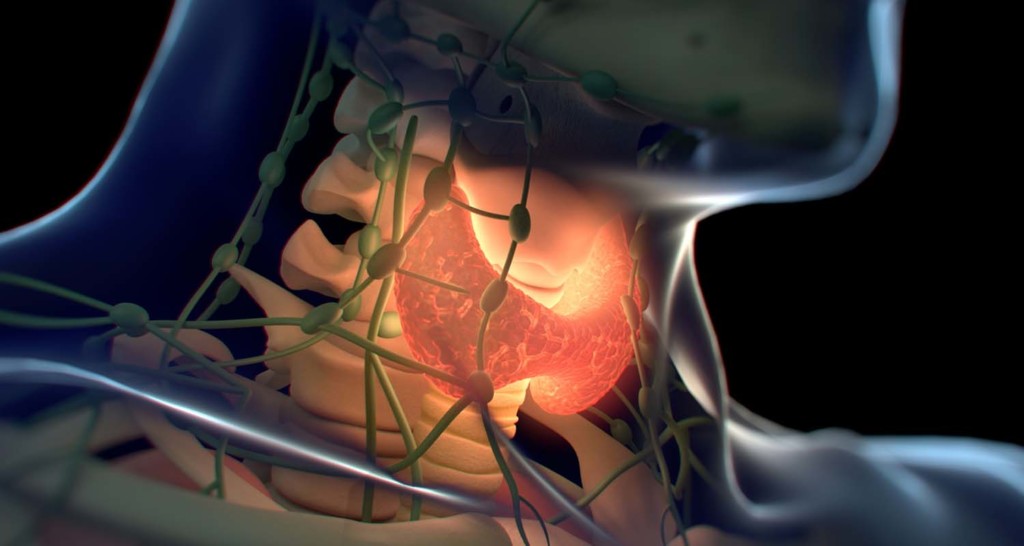
The easier question to answer is, what doesn’t the thyroid do? Your thyroid secretes hormones that regulate pretty much everything your body does, like:
- Menstrual cycles
- Heart function
- Digestion
- Mood
- Bone density
- Brain function
- Metabolism
Those are only a few of them. A complete list of everything the thyroid does would have you scrolling for days. That’s why it’s so crucial that it works, and why it can ruin your life if it doesn’t. Too little thyroid hormone and it feels like your whole body is asleep and you’re carrying a sack of rocks on your back. Too much, and you feel panicky and turbocharged, not in a good way.
Thyroid symptoms
In general, you have a thyroid disorder if your thyroid makes too much or too little hormone.
Hyperthyroidism symptoms
Hyperthyroid is an overactive thyroid, when you make too much thyroid hormone. Hyperthyroid symptoms include:
- Anxiety
- Irritability
- Dizziness, vertigo
- Mental problems
- Heart palpitations
- Tremors
- Feeling too hot
- Excess sweat
- Scant or missed periods in women
- Infertility
- Blurred vision
- Weight changes (usually loss)
- Thinning of hair
- Itching
- Rashes
- Possible increase in blood sugar
- Fatigue
Thyroid disorders that cause hyperthyroid
Your thyroid can work overtime for various reasons.
Graves’ disease. Graves’ disease is an autoimmune condition where your immune system attacks the thyroid. Instead of destroying the tissue, it binds to thyroid receptors which activates hormone production. Then, it floods your body with too much hormone.
Subacute thyroiditis. When your thyroid gland is inflamed, thyroid hormone can seep out. This form of hypothyroidism is temporary — usually, it lasts only a few weeks.
Hypothalamus and pituitary miscommunications. When the hypothalamus detects low thyroid hormone levels, it releases thyrotropin-releasing hormone (TRH), which tells the pituitary gland to release thyroid stimulating hormone (TSH). TSH then tells the thyroid to ramp up thyroid hormone production. When one of these misfires, you don’t make the right amount of thyroid hormone.
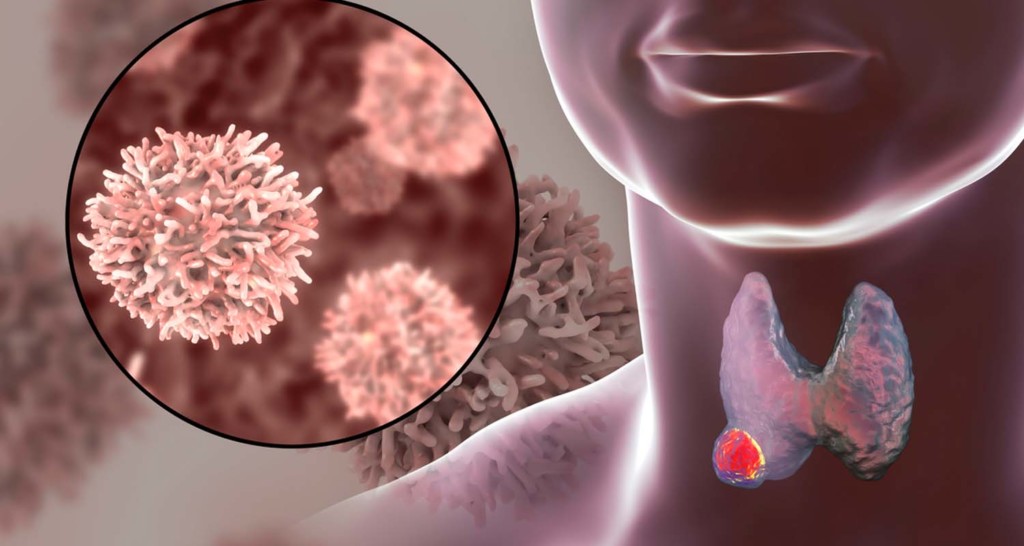
Adenomas, or nodules. When bumps develop on the thyroid, they can become active and secrete thyroid hormone. Nodules can be benign or cancerous, so if you have them, get them checked out by your functional medicine doctor.
Thyroid cancer. Thyroid cancer can cause hyperthyroidism, or it can decrease thyroid function and cause hypothyroid symptoms.
Hypothyroidism symptoms

Hypothyroid is the opposite of hyperthyroid — your thyroid doesn’t make enough hormone. Hypothyroid symptoms include:
- Weight gain
- Hair loss
- Dry skin
- Dry hair that’s prone to breakage
- Pale skin
- Cold intolerance
- Fatigue
- Weakness
- Constipation
- Depression
- Irritability
- Memory problems
- Heavy or erratic periods
- Decreased libido
One lesser known but common symptom is that you lose the outer third of your eyebrows. I probably had thyroid problems as a kid, because I still have thin outer eyebrows.
Thyroid disorders that cause hypothyroid

There are several reasons why you don’t get enough thyroid hormone.
Toxic load. If your body’s detox systems like the liver and kidneys have too much to deal with, you might not be getting rid of all of the toxins you come into contact with on a daily basis. That’s when autoimmune disease develops, and sometimes, the thyroid is the target. Which brings us to…
Hashimoto’s thyroiditis. Hashimoto’s, aka lymphocytic thyroiditis, is an autoimmune disease of the thyroid, which means the immune system somehow marked the thyroid as an invader and attacks it. Tissues get damaged, and it doesn’t produce enough thyroid hormone.
Certain prescriptions. Some medications slow thyroid function. Ask your doctor or pharmacist if any medicines you take are concerning.
You no longer have a thyroid gland. If you’ve had surgery to remove the thyroid or part of it, or if your doctor killed off your thyroid with radiation because you made too much hormone, you might not make sufficient thyroid hormone or any at all.
Radiation. If you’ve had radiation treatments on or near the neck for cancer, your thyroid might have been damaged in the crossfire. That would affect how much hormone your thyroid makes.
Iodine deficiency. Your thyroid needs iodine to work properly, and you have to get it through your diet. Your doctor might tell you that iodine deficiency is rare in the US, but that’s not a reason to skip a test. Food manufacturers add iodine to things like bread, milk, packaged foods, and table salt. If you’ve adopted a diet that keeps inflammation down, you’re not eating any of those things, so you’re not getting added iodine. That’s not a reason to reach for a loaf of sandwich bread. You can get a well-sourced supplement iodine if you’re deficient and keep eating real food.
Pregnancy and postpartum. Some women experience postpartum thyroiditis, inflammation in the thyroid sometime in the first year after having a baby. Thyroid hormone production increases, then drops, causing symptoms. It’s usually temporary, but have your doc keep an eye on it.
Congenital hypothyroidism. Some people are born with a bum thyroid. Congenital hypothyroidism is when the thyroid didn’t develop properly. Most hospitals screen for it at birth.
Hypothalamus or pituitary abnormalities. Your hypothalamus releases thyrotropin-releasing hormone (TRH), which tells the pituitary gland to release thyroid stimulating hormone (TSH). When the hypothalamus doesn’t make enough TRH, your pituitary gland doesn’t release enough TSH and your thyroid doesn’t get the message to produce hormone. Or, the hangup can happen at the pituitary level, and it doesn’t release enough TSH. Either way, you need enough of both to keep everything communicating and functioning.
Thyroid tests and thyroid optimal ranges — what to expect at the doctor

Chances are, you’ve landed here and you’re reading this because you’re having a heck of a time navigating thyroid testing and diagnosis. Maybe you know something’s up, but your tests are coming back normal, or you feel like you’re not getting the full picture.
You’re not alone. If you’re going to a western medicine doctor for thyroid symptoms, you might have some back and forth, even some second or third opinions before you get the information you need.
Functional medicine and naturopathic doctors are simply better at diagnosing and treating the thyroid. The difference lies in the tests ordered and what’s considered “normal.” There are exceptions — doctors are out there who fully understand how hormone levels, blood tests, medications, and individual differences between patients all work. But, you’ll need to do some digging to find “Dr. Right,” as Bulletproof Radio podcast guest Izabella Wentz (The Thyroid Pharmacist) calls them. (iTunes)
When they’re licensed in your state, functional medicine and naturopathic doctors can order all of the blood tests and prescriptions you might need, and they’re likely to incorporate non-medical interventions as well.
A lot of docs will use TSH only as in the indicator of your thyroid function. If that’s the case, you might want to go doctor shopping.
Here are the thyroid tests that will give you the full picture of how everything’s working:
- TSH
- Free T4
- Free T3
- Reverse T3
- Thyroid Peroxidase Antibodies (TPOAb)
- Thyroglobulin Antibodies (TgAb)
TSH – Thyroid Stimulating Hormone
TSH is the hormone that tells your thyroid to make more thyroid hormone. Here’s how it works.
Your hypothalamus is like the thermostat for thyroid hormone — it keeps watch on how much thyroid hormone is in your bloodstream, and it responds when you need more. When your level drops too low, it releases TRH, thyroid releasing hormone. Your pituitary gland picks up on TRH, and it releases TSH in response.
Does it test thyroid function? Well, yes, but only if your hypothalamus and pituitary are doing their thing. The stops on the signaling pathway can get messed up for various reasons. Any problems with detecting hormone or releasing hormone at any point in the cascade, and the TSH test becomes worthless.
TSH Optimal range: 0.5-2 IU/L
High TSH
High TSH indicates you’re hypothyroid. Since it’s a signaling hormone, high TSH indicates that your body detects low hormone, so it’s turning up the volume on the signal to make more. If your thyroid isn’t or cannot respond because it’s compromised in some way, you’ll produce more and more TSH. This number can really go off the charts, depending on how low you are and how long you’ve been hypothyroid.
Low TSH
Low TSH tells you that you have too much thyroid hormone, or that you can cut your dose of thyroid medication, so it indicates hyperthyroid. Certain thyroid medications can suppress your TSH, so if you don’t have symptoms you’re still in good shape.
Normal TSH
On one hand, normal TSH could mean that your thyroid is fine. On the other hand, you can have a normal number for TSH and still have an abnormal thyroid. One lab’s normal differs from the next, one doctor’s optimal ranges differ from the next. You can’t rely on TSH alone to tell how your thyroid is doing, especially if you have symptoms.
Free T4 – Thyroxine
Your thyroid makes mostly T4, also known as thyroxine. Thyroxine is the storage form of thyroid hormone — it circulates in the bloodstream, then your tissues snap it up and store it. When an area of your body needs a power boost, it gets converted into the active form, T3 (more on that in a minute). Most of it is bound to protein in the blood, but free T4 is unbound and available for your body to use.
Optimal Free T4 range: 15-23 pmol/L
High Free T4 indicates hyperthyroidism.
Low Free T4 indicates hypothyroidism.
T3 – Triiodothyronine
When your tissues determine they need a power-up, they convert T4 into Free T3, the active form of thyroid hormone. Sometimes your thyroid makes sufficient hormone, but you don’t convert it, so you’ll get hypothyroid symptoms.
Optimal Free T3 range: > 5-7 pmol/L
High Free T3 indicates hyperthyroidism
Low Free T3 might explain hypothyroid symptoms. If your Free T4 is fine and your Free T3 is low, you might have trouble converting T4 to T3.
Reverse T3
Some of your T4 stores convert to Reverse T3. While T3 helps your cells make energy, Reverse T3 slows down T3 and slows down energy production. You might think more energy is better, but if your cells make too much energy, you end up with hyperthyroid symptoms like racing heart and anxiety.
Optimal reverse T3 range: 11-18 ng/dl
High Reverse T3 might explain hypothyroid symptoms. A high number indicates your body is using too much T4 to make Reverse T3, and not making enough Free T3 that your cells use to make energy.
Low Reverse T3 might explain hyperthyroid symptoms. If you don’t have enough of it and your other thyroid hormones are within range, your cells are making too much energy and you feel it — not in a good way.
Thyroid Antibodies — TPOAb and TgAb
TPOAb — Thyroid Peroxidase Antibodies Thyroid peroxidase antibodies attack the enzyme used to make thyroid hormone.
TgAb — Thyroglobulin Antibodies Thyroglobulin antibodies attack thyroglobulin, which your thyroid uses to make hormone.
If either or both of these antibodies test high, that means your immune system attacks the thyroid. That means you have one of two autoimmune thyroid diseases — Hashimoto’s thyroiditis if you’re hypothyroid, and Graves’ disease if you’re hyperthyroid.
Optimal thyroid antibodies range (either TPOAb or TgAb): < 2 IU/m
Your thyroid uses iodine to make thyroid hormones. If you don’t have enough, you don’t make enough hormone, and you’ll have hypothyroid symptoms.
Your doctor will probably tell you that iodine deficiency is rare. That might have been true when everyone was eating white sandwich bread and conventional iodized salt. If you’re eating a real-food diet that keeps inflammation down, you’re probably not getting iodine that food manufacturers put into foods.
There are a few ways to test. One way to test at home is to draw a 2 inch square on your forearm with a non-toxic pen, and “paint” on a 2% iodine solution. Be careful not to wash it off! If it fades before the 24-hour mark, ask your doctor to test your iodine levels.
You can only know for sure if a lab measures your levels. If you’re getting tests done anyway, ask to tack on the iodine test.
Iodine Optimal iodine levels — >100 µg/L (urine test)
If you’re low and you do supplement, make sure the supplement you choose is a high-quality kelp iodine supplement that comes from waters with low levels of heavy metals.
Thyroid medication and treatment

Hypothyroid medication and treatment
When I found out I had Hashimoto’s, I had to go on thyroid medication to get enough thyroid hormone. The most common medication that doctors prescribe for hypothyroid is Synthroid, which contains T4 only. Other T4 only medications include Tirosint and Levoxyl. That will work for you if you’re converting T4 to T3, but it won’t do a thing for you if you if your problem lies with conversion.
People with conversion problems will feel better on combination T4/T3 medications like Nature-Throid, Armour, or a custom-compounded formula.
Less commonly, doctors will prescribe a T3-only thyroid medication, like Cytomel.
Hyperthyroid medication and treatment
When you have too much thyroid hormone, there are a few ways to tackle it.
Anti-thyroid medication. Anti-thyroid medication keeps your thyroid from making hormone.
Radioactive iodine. The thyroid absorbs iodine, but the rest of the body doesn’t. So, by using radioactive iodine, you can selectively damage thyroid cells with radiation, and prevent them from making hormone. The damage is permanent. The risk is going overboard, causing an underactive thyroid and requiring a lifetime of thyroid medication.
Surgery. You can get all or part of the thyroid gland removed. Or, the surgeon could remove an active nodule that secretes hormone.
On an episode of Bulletproof Radio (iTunes), I talked with thyroid expert Dr. Izabella Wentz, PharmD, about her protocol. She focuses on building the body’s natural resilience by zeroing in on natural defense systems, like the liver.
“I started thinking about what are the fundamentals of healing for each person. What are the things that just about everybody can do to make themselves feel better regardless of what their root cause is, because every Hashimoto’s patient is like a snowflake, everybody’s got a slightly different story. But supporting our own body’s natural protective defenses, supporting the liver, helps to build resilience, because now, we’re no longer toxic to everything.”
Getting your body working properly might help your thyroid work again, or lessen your medication.
When I went on SARMs, I started getting hyperthyroid symptoms, so I went off of my medication. After a few months, I noticed low-thyroid symptoms like brittle hair and hair loss, so I went back on but I adjusted my dose. With the extra muscle mass, I had more mitochondria, so I was making enough energy to avoid the energy dips, but I still didn’t have enough thyroid hormone. Any doctor would tell you that there’s no moral victory for going off of thyroid medication if you need it.
Okay, I threw a lot of info at you. The point is not for you to become a thyroid expert. Instead, use this information to have an informed conversation with your doctor about your symptoms, your testing, and how it all fits together.
The most common thyroid story I hear is the one where a person was in and out of the doctor’s office several times before someone finally pinpointed the right testing and treatment plan. Having a basic understanding can help you ask the right questions and better yet, find the right doctor who understands what you’re going through and how to approach it.