[tldr]
- Although fungal acne has come onto the scene as a relatively new discussion, it’s not a new condition.
- Fungal acne looks a lot like hormonal acne or bacterial acne, but the culprit isn’t the same as other types of acne. Instead, it is an overgrowth of yeast that hangs around in the hair follicles.
- Researchers have observed fungal acne crop up after events that compromise the immune system, such as certain illnesses, transplants, etc. among other causes. Or, fungal acne can occur without a major event that weakens the immune system.
- Here’s how to identify fungal acne, and what to do about it.
[/tldr]
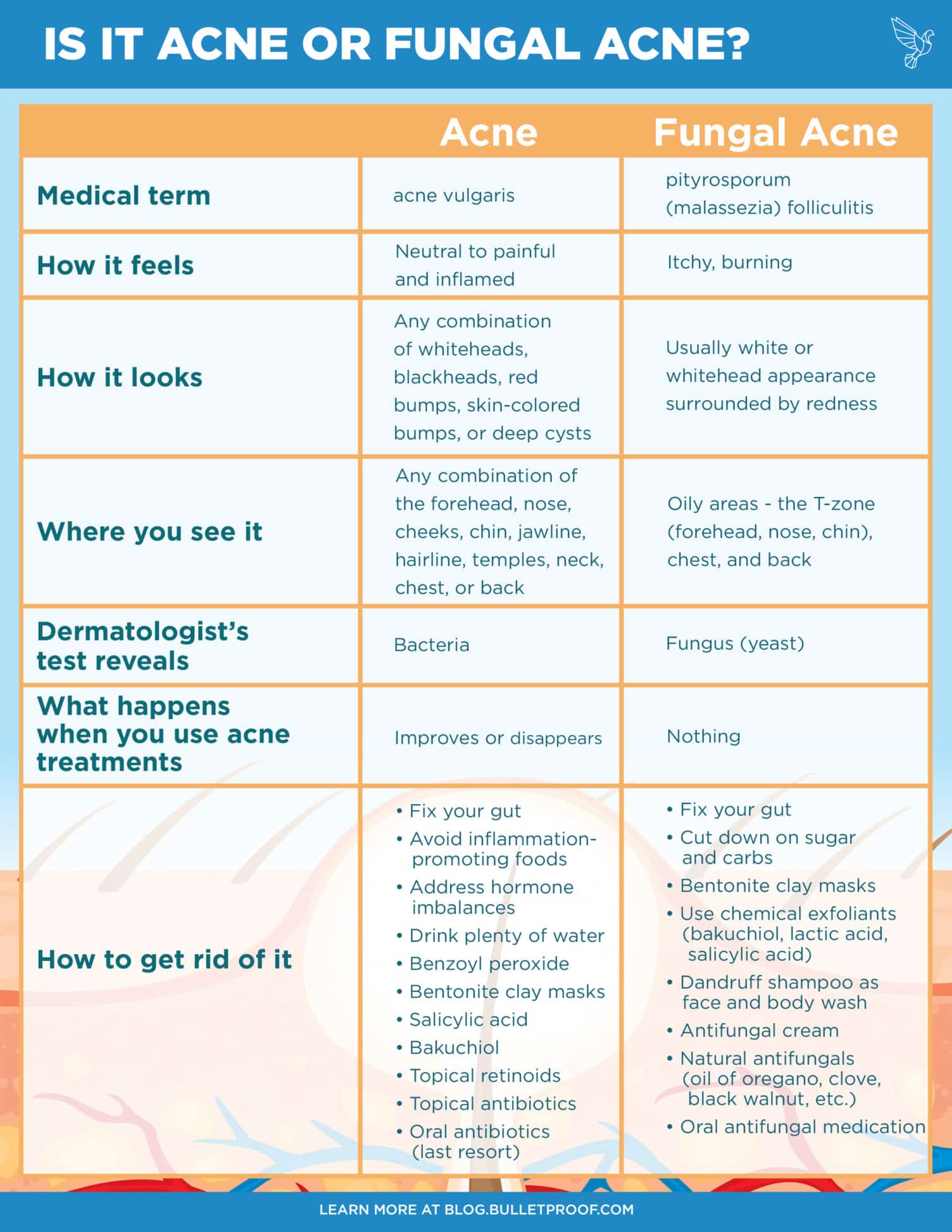
If you have breakouts that won’t budge, no matter what treatments you try, you could be dealing with fungal acne. Although the term fungal acne might be new to you, it’s not a new condition. In fact, it’s not even really acne. That’s why you can put all the benzoyl peroxide and salicylic acid you want on fungal acne, and it won’t disappear. Here’s what you need to know about fungal acne, including what it looks like and how to treat it, so you can figure out once and for all what kind of acne you’re dealing with — and get back to clear, radiant skin.
What is fungal acne?
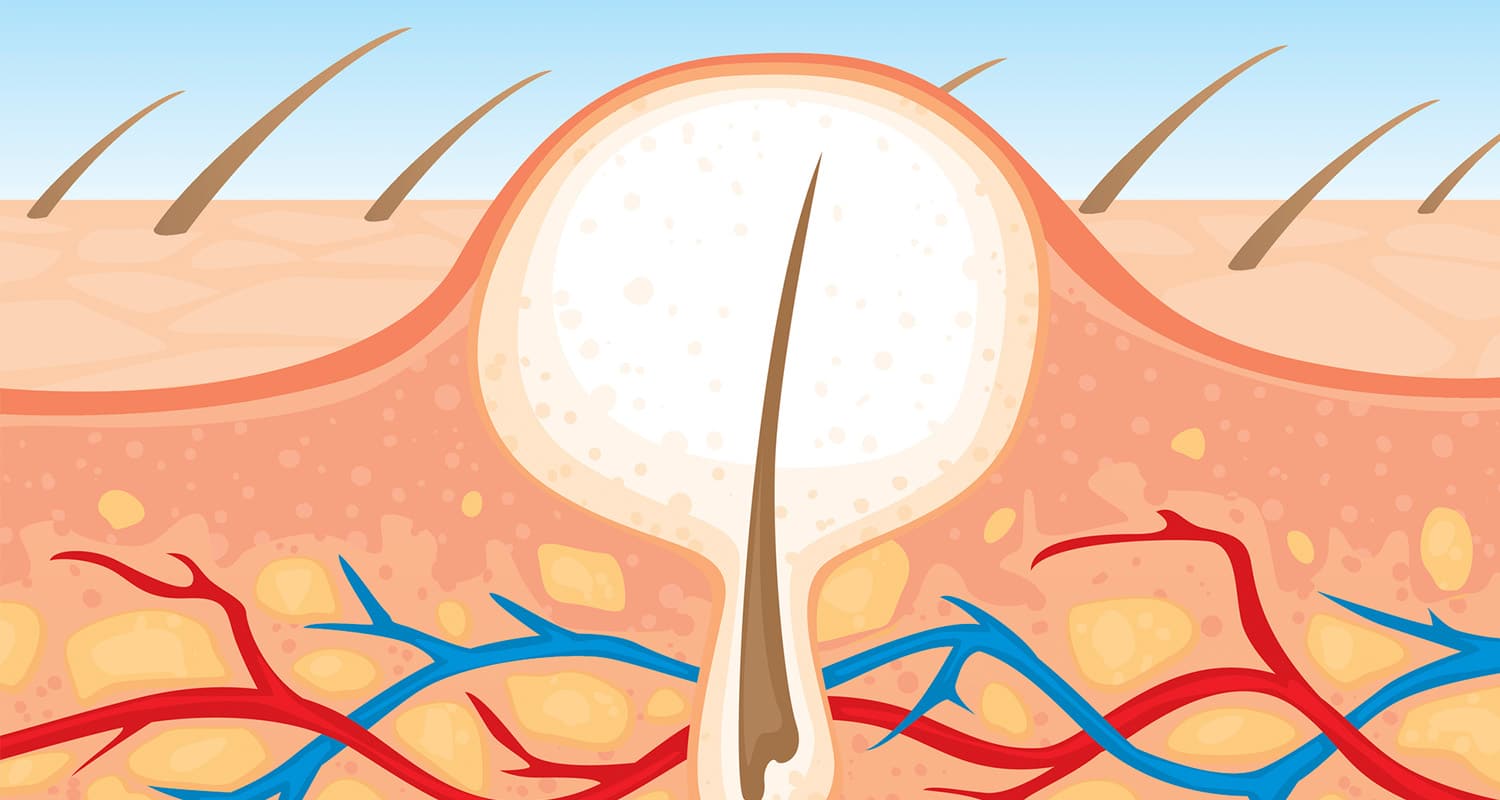
Fungal acne looks a lot like hormonal acne or bacterial acne, but the culprit isn’t the same as other types of acne. Instead, it is an overgrowth of yeast that hangs around in the hair follicles. The technical term: pityrosporum folliculitis or malassezia folliculitis.
Fungal acne appears as inflamed, itchy, acne-like eruptions that are really pus-filled bumps. It shows up as breakouts in areas where you typically have a lot of oil — in your T-zone (forehead, nose, chin), chest and back. The telltale difference is that fungal acne can be itchy, and regular acne is not. Other clues: fungal acne is generally uniform in size and shape, and appears in clusters of small whiteheads.
Fungal acne is especially frustrating to treat, because it looks so much like regular acne (which is caused by bacteria). Just as you can’t attack a cold virus with antibiotics and expect to get better, you can’t treat fungal acne with traditional acne medications. The good news is, once you know what you’re dealing with and use the proper treatments, you’ll see massive improvements in your complexion.
What causes pityrosporum (malassezia) folliculitis?
Malassezia, the yeast responsible for fungal acne, lives on everyone’s skin. It’s only when its balance is thrown out of whack that an outbreak occurs. Pityrosporum folliculitis stems from a range of imbalances.
Your skin microbiome, the balance of beneficial and troublesome microorganisms on your skin, can shift from changes in your diet, environment, medication, workout regimen, skincare routine, or dozens of other reasons. Sometimes it will rebalance itself, and other times, you’ll need to step in to help it along. Yeasts love warm, wet environments, so keeping skin dry and clean during workouts and after can help. Yeasts also love sugar and carbs, so you may notice improvement after cutting back on sweets.
Not every instance of fungal acne gets scientifically investigated, but folliculitis that follows specific medical conditions grabs scientists’ attention. Researchers also have observed fungal acne crop up:
- After taking antibiotics[ref url=”https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2133.1973.tb08015.x”][ref url=”https://jamanetwork.com/journals/jamadermatology/article-abstract/530748″]
- If you have HIV and AIDS[ref url=”https://jamanetwork.com/journals/jamadermatology/article-abstract/552692″][ref url=”https://www.jaad.org/article/S0190-9622(86)70126-6/abstract”][ref url=”https://europepmc.org/abstract/med/10417509″]
- After spending time in intensive care[ref url=”https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-4362.1999.00718.x”]
- After transplant surgery,[ref url=”http://annals.org/aim/article-abstract/701374/pityrosporum-folliculitis-after-bone-marrow-transplantation-clinical-observations-five-patients”][ref url=”https://www.sciencedirect.com/science/article/pii/S1053249899001230″][ref url=”https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1346-8138.2000.tb02118.x”][ref url=”http://awarticles.s3.amazonaws.com/8965683.pdf”] Note: patients take immunosuppressants after transplants so the common thread seems to be a weakened immune system[ref url=”https://onlinelibrary.wiley.com/doi/full/10.1111/j.1439-0507.2009.01814.x”]
Or, you could have fungal acne without having experienced any of these. There are plenty of conditions that create the ideal environment for fungal acne that scientists haven’t investigated yet.
The immune system connection is worth paying attention to. Your skin has its own microbiome, an ecosystem of microorganisms that benefit your skin in the right balance, or disrupt your skin’s function when the wrong species take over. Your microbiome is a crucial part of your immune system and helps your body fight off the pathogens that cause problems.
Restoring a disrupted balance of flora involves a multi-step process and antifungals might be a quicker fix, but to keep fungal acne away long-term, you have to pay attention to your beneficial bacteria. More on that coming up.
How to know for sure that you have fungal acne
A few things can clue you in that you’re dealing with fungal acne:
- Your acne doesn’t respond to over-the-counter or prescription acne treatments, or they make the problem worse
- Your acne feels itchy or burns to the touch
- You have other signs of fungal overgrowth, like dandruff, tinea versicolor, psoriasis, eczema, etc.
The only way to know for sure whether your acne is fungal or bacterial is to have your dermatologist grab a sample of the surface skin cells and test them. Don’t worry — it takes a few seconds and it’s painless.
While you’re waiting for answers, you can experiment with over-the-counter and natural ways to fight fungus in your body (what to do about it, coming up).
Pityrosporum folliculitis fungal acne treatment
Here’s how to get rid of fungal acne for good.
Outside-in fungal acne treatment
- Use a chemical exfoliant on your skin. This keeps pores clear of dead skin cells, which trap oil and create a buffet table for pityrosporum and yeasts. Look for ingredients like lactic acid, bakuchiol, or salicylic acid.
- Experiment with over-the-counter topical fungus treatments. You may see a difference when you use antifungal creams, or when you use dandruff shampoo as body or face wash.
- Wear natural, breathable fabrics. Synthetic materials can be irritating and contribute to oil production on your chest and back. Make sure oil isn’t trapped, and can dissipate naturally.
- Remove wet workout clothes immediately after exercising.
- See your dermatologist. Ask specifically for testing for fungal acne. A simple test can save you loads of frustration, and you can start the right treatments. You may find that your acne is fungal, bacterial, or a combination of the two.
Inside-out fungal acne treatment
- Cut sugar and go low-carb. Yeasts and fungi love sugar and simple carbs that convert to sugar in your body. If you starve them, they won’t hang around for long.
- Balance your gut microbiome. Your microbiome in your gut balances the microbiome in other parts of your body, including your skin. Keep your gut in balance, and the beneficial organisms everywhere else will stay happy. Listen to this episode of the Bulletproof Radio podcast (iTunes) to learn how to fix your gut. You can use the Viome Gut Intelligence Test to get your gut microbiome analyzed (yes it’s an affiliate, becuase I strongly believe in them. use “DAVE” at checkout for $10 off). Also Just Thrive has probiotics to help balance your gut microbiome.
- Explore natural antifungals. Oregano, clove, black walnut, and other plants are natural antifungals that you can find as capsules or in essential oil form. If you use the essential oils, consult an expert to learn how to use them so you don’t damage your skin — they’re powerful. Caprylic acid, a medium-chain triglyceride with an 8-carbon chain, isn’t appetizing to yeasts — in fact, it combats fungi.
- Ask your dermatologist about oral antifungal medication. After tests have confirmed it is pityrosporum folliculitis, talk to your doctor about what combination of oral and topical medications will work best.
Your skin is an important indicator of what’s happening on the inside. Looking your best on the surface is a clear signal that everything’s working well in your body. It’s your job to figure out where you can make adjustments so that you can look and feel amazing every single day.