[tldr]
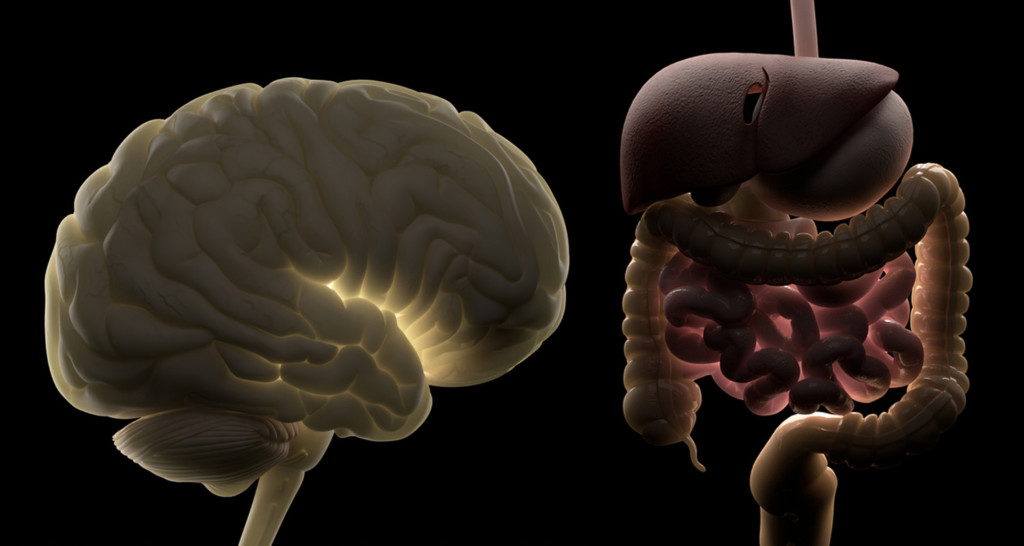
- Your gut and your brain are constantly talking to one another. This communication is known as the gut-brain axis.
- Stress is bad news for the brain-gut axis, and stress signals trigger the release of neurotransmitters and proinflammatory cytokines (molecules that contribute to inflammation and disease).
- Stress can cause various digestive disorders including inflammatory bowel disease (IBS), peptic ulcers, and food allergies.
- Your goal is to control your stress, which in turn will calm your gut. It goes the other way too. By fixing your gut, you’ll feel less stressed.
- An inflamed gut has also been linked to various mood and behavioral disorders including depression, autism, and even neurodegenerative diseases.
- Stomach irritations and gut imbalances send signals to the brain via the central nervous system (CEN), triggering changes in your mood.
- Eating a diet full of anti-inflammatory, nutrient-dense foods is one of the most powerful ways to heal your gut.
[/tldr]
Have you ever felt nauseous when you’ve been worried about something? Or had “butterflies” in your stomach when nervous? The brain sends signals to the gut that produces these physical symptoms.
Scientists are discovering that it goes the other way too — when your gut is inflamed or imbalanced, it sends a signal to your brain. You then feel stressed or worried or depressed. It turns out that your gut and your brain are constantly talking to one another. Learn how this brain-gut communication works, how it impacts your mood and stress levels, and what you can do to control the conversation.
Instantly download Gut Check: Guide to Troubleshooting Your Microbiome to get back in balance fast
The gut-brain axis
The back-and-forth communication between your brain and your gut is known as the gut-brain axis, and occurs primarily along an information superhighway called the vagus nerve. A strong vagus nerve improves the communication between your gut and your brain, so it’s vital that you keep it in working order.
Related: Signs Your Gut Is Unhealthy and Why You Should Fix It
Stress and the gut
Stress is bad news for the brain-gut axis, and stress signals trigger the release of neurotransmitters and proinflammatory cytokines (molecules that contribute to inflammation and disease), which affect the gut in all kinds of ways.[ref url=”https://www.ncbi.nlm.nih.gov/pubmed/22314561 “][ref url=”https://www.ncbi.nlm.nih.gov/pubmed/21040780”] Stress can cause:
- Intestinal dysmotility (when the muscles and nerves of the digestive system don’t work properly)
- Holes in the intestine, allowing toxins, bacteria, and food particles to escape and enter your bloodstream
- An imbalance in your gut bacteria
- Decreased blood flow and oxygenation to the gastrointestinal (GI) tract
- Acid reflux
This digestive damage can develop into serious GI disorders including inflammatory bowel disease (IBS), peptic ulcers, and food allergies.
Your goal is to control your stress, which in turn will calm your gut. It goes the other way too. By fixing your gut, you’ll feel less stressed (more on healing your gut below). Meditation, working out, and sleeping better are all tried-and-true ways to lower stress. Learn more stress management techniques here.
Gut health and mood
You’ve just come off a round of antibiotics, and at the same time you’ve been reaching for sugary foods a little too often. You notice you’re feeling more blah than usual and a bit low. That’s probably no coincidence, thanks again to the gut-brain axis.
A groundswell of research in recent years points to a strong link between what’s going on in your gut and various mood and behavioral disorders including depression, autism, and even neurodegenerative diseases.[ref url=”https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4662178/ “] [ref url=”http://advances.sciencemag.org/content/2/1/e1500997”] [ref url=”https://www.sciencedirect.com/science/article/pii/S0924933816008464 “] [ref url=”https://www.nature.com/articles/mp201650 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3179073/ “] Stomach irritations and gut imbalances send signals to the brain via the central nervous system (CEN), triggering changes in your mood.
Related: How Your Gut Bacteria Control Your Mind
A recent study found that transferring the fecal bacteria of depressed people to rats led to depressed behavior in the rats.
Another study divided 40 healthy women into two groups based on their gut bacteria composition (this after analyzing the women’s stools). The women with a prevalence of one type of bacteria reported feeling less anxious, stressed, and irritable after looking at negative images compared to the other group, whose guts were dominated by a different kind of bacteria. Scans also showed differences in the women’s brains — those who said they felt less stressed showed lower brain volume in areas like the hippocampus than the other group.[ref url=”https://journals.lww.com/psychosomaticmedicine/Citation/2017/10000/Brain_Structure_and_Response_to_Emotional_Stimuli.10.aspx”]
Related: New Research Links Mental Illness and Inflammation. Here’s What You Need to Know
How to fix your gut
Eating a diet full of anti-inflammatory, nutrient-dense foods is one of the most powerful ways to heal your gut. Get more gut-friendly diet tips here, as well as other ways to fix your gut. And if you’re looking to lose weight, learn more about the connection between gut bacteria and weight loss here.